50 years of fraud
 Until the second world war, hypothyroidism was diagnosed on the basis of BMR (basal metabolic rate) and a large group of signs and symptoms. In the late 1940s, promotion of the (biologically inappropriate) PBI (protein-bound iodine) blood test in the U.S. led to the concept that only 5% of the population were hypothyroid, and that the 40% identified by “obsolete” methods were either normal, or suffered from other problems such as sloth and gluttony, or “genetic susceptibility” to disease. During the same period, thyroxine became available, and in healthy young men it acted “like the thyroid hormone.” Older practitioners recognized that it was not metabolically the same as the traditional thyroid substance, especially for women and seriously hypothyroid patients, but marketing, and its influence on medical education, led to the false idea that the standard Armour thyroid USP wasn’t properly standardized, and that certain thyroxine products were; despite the fact that both of these were shown to be false.
Until the second world war, hypothyroidism was diagnosed on the basis of BMR (basal metabolic rate) and a large group of signs and symptoms. In the late 1940s, promotion of the (biologically inappropriate) PBI (protein-bound iodine) blood test in the U.S. led to the concept that only 5% of the population were hypothyroid, and that the 40% identified by “obsolete” methods were either normal, or suffered from other problems such as sloth and gluttony, or “genetic susceptibility” to disease. During the same period, thyroxine became available, and in healthy young men it acted “like the thyroid hormone.” Older practitioners recognized that it was not metabolically the same as the traditional thyroid substance, especially for women and seriously hypothyroid patients, but marketing, and its influence on medical education, led to the false idea that the standard Armour thyroid USP wasn’t properly standardized, and that certain thyroxine products were; despite the fact that both of these were shown to be false.
By the 1960s, the PBI test was proven to be irrelevant to the diagnosis of hypothyroidism, but the doctrine of 5% hypothyroidism in the populaton became the basis for establishing the norms for biologically meaningful tests when they were introduced.
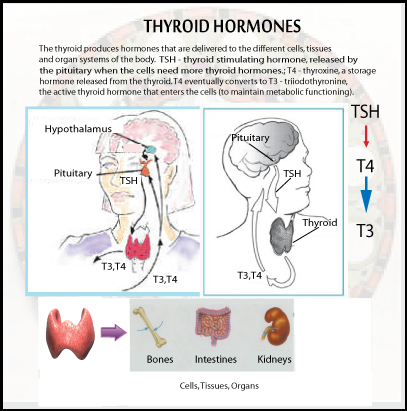
Meanwhile, the practice of measuring serum iodine, and equating it with “thyroxine the thyroid hormone,” led to the practice of examining only the iodine content of the putative glandular material that was offered for sale as thyroid USP. This led to the substitution of materials such as iodinated casein for desiccated thyroid in the products sold as thyroid USP. The US FDA refused to take action, because they held that a material’s iodine content was enough to identify it as “thyroid USP.” In this culture of misunderstanding and misrepresentation, the mistaken idea of hypothyroidism’s low incidence in the population led to the acceptance of dangerously high TSH (thyroid stimulating hormone) activity as “normal.” Just as excessive FSH (follicle stimulating hormone) has been shown to have a role in ovarian cancer, excessive stimulation by TSH produces disorganization in the thyroid gland.
Tests & the “free hormone hypothesis”
After radioactive iodine became available, many physicians would administer a dose, and then scan the body with a Geiger counter, to see if it was being concentrated in the thyroid gland. If a person had been eating iodine-rich food (and iodine was used in bread as a preservative/dough condition, and was present in other foods as an accidental contaminant), they would already be over saturated with iodine, and the gland would fail to concentrate the iodine. The test can find some types of metastatic thyroid cancer, but the test generally wasn’t used for that purpose. Another expensive and entertaining test has been the thyrotropin release hormone (TRH) test, to see if the pituitary responds to it by increasing TSH production. A recent study concluded that “TRH test gives many misleading results and has an elevated cost/benefit ratio as compared with the characteristic combination of low thyroxinemia and non-elevated TSH.” (Bakiri, Ann. Endocr (Paris) 1999), but the technological drama, cost, and danger (Dokmetas, et al., J Endocrinol Invest 1999 Oct; 22(9): 698-700) of this test is going to make it stay popular for a long time. If the special value of the test is to diagnose a pituitary abnormality, it seems intuitively obvious that overstimulating the pituitary might not be a good idea (e.g., it could cause a tumor to grow).
Everything else being equal, as they say, looking at the amount of thyroxine and TSH in the blood can be informative. The problem is that it’s just a matter of faith that “everything else” is going to be equal. The exceptions to the “rule” regarding normal ranges for thyroxine and TSH have formed the basis for some theories about “the genetics of thyroid resistance,” but others have pointed out that, when a few other things are taken into account, abnormal numbers for T4, T3, TSH, can be variously explained.
The actual quantity of T3, the active thyroid hormone, in the blood can be measured with reasonable accuracy (using radioimmunoassay, RIA), and this single test corresponds better to the metabolic rate and other meaningful biological responses than other standard tests do. But still, this is only a statistical correspondence, and it doesn’t indicate that any particular number is right for a particular individual.
Therapy
Years ago it was reported that Armour thyroid, U.S.P., released T3 and T4, when digested, in a ratio of 1:3, and that people who used it had much higher ratios of T3 to T4 in their serum, than people who took only thyroxine. The argument was made that thyroxine was superior to thyroid U.S.P., without explaining the significance of the fact that healthy people who weren’t taking any thyroid supplement had higher T3:T4 ratios than the people who took thyroxine, or that our own thyroid gland releases a high ratio of T3 to T4. The fact that the T3 is being used faster than T4, removing it from the blood more quickly than it enters from the thyroid gland itself, hasn’t been discussed in the journals, possibly because it would support the view that a natural glandular balance was more appropriate to supplement than pure thyroxine.
Diagnosis
In the absence of commercial techniques that reflect thyroid physiology realistically, there is no valid alternative to diagnosis based on the known physiological indicators of hypothyroidism and hyperthyroidism. The failure to treat sick people because of one or another blood test that indicates “normal thyroid function,” or the destruction of patients’ healthy thyroid glands because one of the tests indicates hyperthyroidism, isn’t acceptable just because it’s the professional standard, and is enforced by benighted state licensing boards.
Toward the end of the twentieth century, there has been considerable discussion of “evidence-based medicine.” Good judgment requires good information, but there are forces that would over-rule individual judgment as to whether published information is applicable to certain patients. In an atmosphere that sanctions prescribing estrogen or insulin without evidence of an estrogen deficiency or insulin deficiency, but that penalizes practitioners who prescribe thyroid to correct symptoms, the published “evidence” is necessarily heavily biased. In this context, “meta-analysis” becomes a tool of authoritarianism, replacing the use of judgment with the improper use of statistical analysis.
Unless someone can demonstrate the scientific invalidity of the methods used to diagnose hypothyroidism up to 1945, then they constitute the best present evidence for evaluating hypothyroidism, because all of the blood tests that have been used since 1950 have been.shown to be, at best, very crude and conceptually inappropriate methods.
Thomas H. McGavack’s 1951 book, The Thyroid, was representative of the earlier approach to the study of thyroid physiology. Familiarity with the different effects of abnormal thyroid function under different conditions, at different ages, and the effects of gender, were standard parts of medical education that had disappeared by the end of the century. Arthritis, irregularities of growth, wasting, obesity, a variety of abnormalities of the hair and skin, carotenemia, amenorrhea, tendency to miscarry, infertility in males and females, insomnia or somnolence, emphysema, various heart diseases, psychosis, dementia, poor memory, anxiety, cold extremities, anemia, and many other problems were known reasons to suspect hypothyroidism. If the physician didn’t have a device for measuring oxygen consumption, estimated calorie intake could provide supporting evidence. The Achilles’ tendon reflex was another simple objective measurement with a very strong correlation to the basal metabolic rate. Skin electrical resistance, or whole body impedance wasn’t widely accepted, though it had considerable scientific validity.
A therapeutic trial was the final test of the validity of the diagnosis: If the patient’s symptoms disappeared as his temperature and pulse rate and food intake were normalized, the diagnostic hypothesis was confirmed. It was common to begin therapy with one or two grains of thyroid, and to adjust the dose according to the patient’s response. Whatever objective indicator was used, whether it was basal metabolic rate, or serum cholesterol. or core temperature, or reflex relaxation rate, a simple chart would graphically indicate the rate of recovery toward normal health.
© Ray Peat 2006. All Rights Reserved. www.RayPeat.com
SOURCE: http://raypeat.com/articles/articles/thyroid.shtml